Remote Patient Monitoring & the Future of Healthcare
Remote Patient Monitoring: A shot in the arm for the future of health care
When Troy Bird started experiencing shortness of breath, fatigue, vomiting, and loss of taste last spring, of course COVID-19 sprang to mind. Concerned with his symptoms, Troy’s wife drove him to the MetroHealth ER in Cleveland. Even though he tested negative for COVID-19 in the ER, the hospital still wanted to keep an eye on Troy’s symptoms once he left. He is a cancer survivor, which puts him at risk for the virus. So, as part of its Hospital at Home program, MetroHealth set up Troy with a remote patient monitoring (RPM) kit.
RPM is one of the telehealth services that has had the greatest impact on health care during the COVID-19 pandemic. According to the Centers for Disease Control and Prevention (CDC), telehealth use rose by 50% in just the first quarter of 2020 and 154% in the last week of March 2020 alone compared with the same period in 20191. While telehealth has been an important tool in maintaining connection to healthcare professionals during the pandemic, doctors seeing patients over a video link are missing data that would normally be collected in person. Remote patient monitoring equipment allows providers to collect this important information through near real-time monitoring of blood oxygenation, heart rate, temperature, respiration rate, blood pressure, and more, while still meeting with the patients remotely.
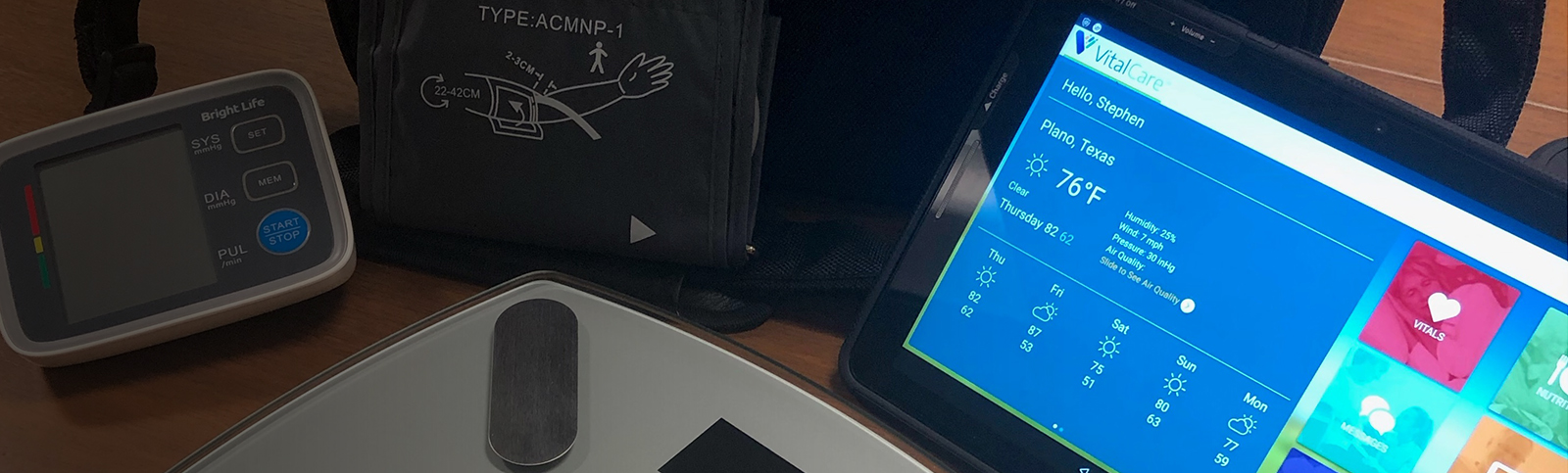
Connectivity is key to RPM and virtual care. We work with virtual connected care providers to provide a highly secure connection for ready-to-use RPM kits. The MetroHealth RPM kits, for example, include an AT&T tablet that uses FirstNet® - the only nationwide, high-speed broadband communications platform dedicated to and purpose-built for America’s first responders and the extended public safety community.* The tablet connects through Bluetooth with the thermometer, blood pressure cuff, and oximeter in the RPM kit to monitor patients’ vitals.
“The COVID pandemic emphasized the value and importance of telehealth delivered care services during a time of crisis and uncertainty,” said Albert Ferreira, director, Telehealth Operations at The MetroHealth System. “During a critical period when in-person care options were very limited, our remote patient monitoring solution and devices allowed us to maximize our clinical resources, minimize staff exposure, and meet the timely care needs of our lower acuity COVID-19 patients from the safety and comfort of their homes.”
For Troy Bird, the use of the RPM kit with daily video telehealth exams with MetroHealth doctors and nurses provided peace of mind.
“My vitals were taken three times a day and transmitted back to MetroHealth Hospital,” said Bird. “I had video calls with the nurse twice a day and with my doctor once a day to discuss the findings. I was very impressed with the whole set-up. Knowing I was monitored throughout the day gave me assurance. And it’s a hundred times easier than driving to see a doctor. I’d definitely be comfortable using a remote patient monitoring kit again.”
Bird is not alone in that sentiment. A 1-year COVID-19 remote patient monitoring pilot launched by the Defense Health Agency2 last September shows patients’ willingness to use remote patient monitoring. As of February 2021, the COVID-19 RPM program had served 98 patients. Twenty-six of those 98 patients returned to a military medical treatment facility or ER for higher levels of care. Of those 26, 73% (19) asked to be re-enrolled in the pilot after their readmission discharge from the hospital. And when consumers were asked in a 2019 Consumer Technology Association survey3, well before the pandemic, if they would use a connected health device if it was recommended by a physician, 52% said they would.
Dr. Anitha Mullangi, chief medical officer at St. John’s Well Child and Family Center in south Los Angeles, understands why.
“It’s convenient for the patients and gives them reassurance knowing someone’s monitoring their vitals and will follow up with them if something goes wrong.”
St. John’s Well Child hadn’t used remote patient monitoring prior to COVID-19. But when the pandemic struck, many of the people served by the nonprofit’s community health clinics were among the hardest hit. For the last six months, St. John’s Well Child used about 200 RPM kits with AT&T wireless connectivity to monitor the oxygen levels and temperature of COVID-19 patients living below the poverty line. Dr. Mullangi is also using RPM kits to monitor St. john’s patients who receive COVID-19 infusion therapy patients – people who receive antibodies from someone who has already had COVID-19. She recognizes the benefits of RPM, especially during a time like the pandemic.
“It frees up staff resources, allows for timely intervention for patient care, and can reduce expenses for providers,” said Mullangi.
Remote patient monitoring also reduces the strain on hospital resources, like in-patient beds, freeing these resources for higher risk or more severe cases.
Dr. Mullangi is optimistic the use of remote patient monitoring will grow, especially if Electronic Health Records systems develop interfaces for telemedicine platforms.
“I can see unlimited possibilities,” Mullangi added.
So can other healthcare providers. As hospitals across the country report increased patient engagement and reduced readmission rates for COVID-19 cases through the use of newly developed RPM programs, some are exploring similar RPM programs for conditions such as cardiovascular disease and cirrhosis. With more health systems and hospitals turning to RPM for improved patient outcomes and reduced costs, GlobalData expects remote patient monitoring to grow significantly.
“A large reason why U.S. hospitals have demonstrated such strong uptake of RPM programs is due to the favorable regulatory and reimbursement changes that the FDA and Centers for Medicare & Medicaid Services have put in place during the pandemic. Our expectation is that the U.S. government will continue to support RPM usage, due to increased patient engagement and care efficiency, which is expected to support the 18% market growth over the next 5 years,” says Dr. David Brown, senior healthcare analyst at GlobalData.
Doctors weren’t strangers to remote patient monitoring before COVID-19. But the pandemic has demonstrated that the ability to provide RPM must be a core capability for providers going forward. Now that virtual care has become the “new norm,” mobility is expected to play a bigger role in connecting the healthcare of the future.
“As the healthcare industry navigates through a massive digital transformation accelerated by the pandemic, we’re providing solutions that can help providers stay connected, protect and manage data, and communicate and collaborate during this unprecedented time and beyond,” said Joe Drygas, VP of AT&T healthcare solutions. “From remote patient monitoring to temperature screening kiosks to pop-up medical solutions, we’re creating connections that healthcare providers need to thrive.”
*MetroHealth joins FirstNet as an extended primary user - organizations and agencies that could be called on to help support public safety in day-to-day operations and during emergency response. Extended primary use cases vary widely and include healthcare, essential government services, transportation, utilities, and others that operate in support of primary public safety entities. Eligibility for extended primary user status is rigorously reviewed before service is approved to help ensure that FirstNet’s unique capabilities remain dedicated to first responders and those who support them.’
FirstNet and the FirstNet logo are registered trademarks of the First Responder Network Authority. All other marks are the property of their respective owners.
1Koonin LM, Hoots B, Tsang CA, et al. Trends in the Use of Telehealth During the Emergence of the COVID-19 Pandemic – United States, January-March 2020. MMWR Morb Mortal Wkly Rep 2020;69:1595-1599. DOI http://dx.doi.org/10.15585/mmwr.mm6943a3
2The appearance of U.S. Department of Defense (DoD) visual information does not imply or constitute DoD endorsement.
3Consumer Technology Association April 11, 2019 press release: CTA Survey Finds High Demand for Remote Patient Monitoring Devices